It is hard to believe that we are now into a new year, with many wondering what 2024 will bring! We hope you have had the opportunity for a safe and restful break, and are starting to make plans for the year. We are also excitedly planning our calendars for the year for running our pathways courses and attending conferences.
Working in the healthcare field can be amazingly rewarding but it is also demanding. When the caseload goes into overflow and waitlists get shut, the last thing on your mind may be ‘what is the latest evidence’? One study found it took 17 years for research evidence to reach clinical practice1 – a frightening statistic. Whilst this length of time may not be the case to implement all new research, it does highlight the ease of falling into prescription habits, some which could detrimentally impact the client you are working with.
Implementing the latest evidence involves more than skimming an abstract; it requires taking the time to read an article, then critically analyse it, and then to reflect on how to implement it into your practice. It isn’t necessarily realistic to set aside time every week to review the latest articles, so how can EBP be implemented alongside a busy schedule? There are four quick suggestions I’d love to go through with you today:
- Set up to receive the latest research relevant to your practice
- Engage in professional supervision
- Prioritise upskilling
- Attend a journal club
1. Set up to receive the latest research relevant to your practice
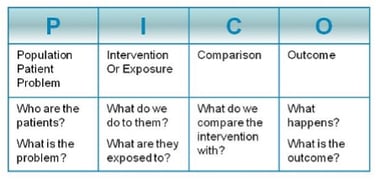 Find a research search engine you would like to use, and complete a search based on your field of interest. Using PICO terms (see image on the right) may be helpful to ensure results are relevant. Once you find a search result that looks useful, request to save the search and have it sent regularly to your emails.
Find a research search engine you would like to use, and complete a search based on your field of interest. Using PICO terms (see image on the right) may be helpful to ensure results are relevant. Once you find a search result that looks useful, request to save the search and have it sent regularly to your emails.
When this comes in, you can skim to see if there is anything of particular interest, and save it for a rainy day.
2. Engage in professional supervision
Supervision is such an important part of developing your skills as a health professional. A supervisor may be internal or external of your organisation, depending on your respective skill sets and needs. Organisations such as the Occupational Therapy Board of New Zealand (OTBNZ) highlight the importance of supervision, including “support for reflective self-assessments which focus on competence”. Reflective practice is such a valuable tool to lead to positive change and development. The OTBNZ provide guidance for what incorporates supervision. “The scope of professional supervision should include:
- input into client care
- professional development and support
- professional accountability”
Having both participated in and facilitated clinical supervision in Australia, one aspect I find particularly valuable is the opportunity it provides for the supervisee to critically reflect on their practice. It can otherwise be easy to keep doing the same things and expecting different results, rather than truly reflecting on and implementing changes. The supervisor then will hopefully also provide further guidance and empowerment to implement these changes, or provide further insights into areas of strengths and learning opportunities. Considering this in relevance to EBP, supervision also provides a space to discuss the method of implementing changes, and reflecting on those outcomes.
3. Prioritise upskilling
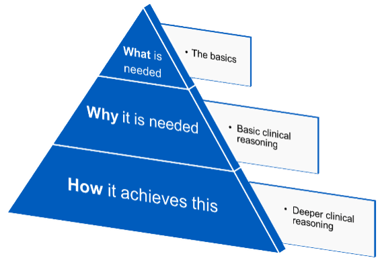
I would encourage you to look for courses that, 1) Have clear learning objectives relevant to you; 2) Update their material and research on a regular basis, and 3) Not only help you in knowing ‘what’ to script (products), but provide deeper clinical understanding of ‘why’ it may be a good solution for a specific circumstance. From there, a deeper learning of the clinical applications, or the ‘how’, is invaluable as you seek to prescribe assistive technology that is functional, evidence-based, and ultimately – used!
4. Attend a journal club
Not everyone finds it easy to sit down and read a whole article. Journal clubs can be a fun and interactive way to discuss an article together, including how to implement any relevant findings. One person will typically provide a mini-presentation on an article, and may prepare some discussion questions for the group.
Sometimes it is difficult to know how to interpret a study, including whether the results are applicable to those whom you work with. A journal club can provide a time to have these discussions and keep up-to-date on current research. If you are interested in running a journal club for the first time, Monash Health put together a resource which may be beneficial.
 I hope you might make some of these a 2024 New Year’s resolution – and one that is kept. No matter our intentions and plans, ultimately it comes down to the priority that evidence-based practice is given in your workplace, and to you yourself as a therapist.
I hope you might make some of these a 2024 New Year’s resolution – and one that is kept. No matter our intentions and plans, ultimately it comes down to the priority that evidence-based practice is given in your workplace, and to you yourself as a therapist.
Author

Roseanna Tegel, BHthSc/ MOT
Clinical Services Specialist
Roseanna Tegel joined Permobil in May 2023 as a Clinical Services Specialist. She graduated from Western Sydney University in 2016 with a Bachelor of Health Science/Master of Occupational Therapy and received the Prize in Undergraduate Occupational Therapy for Overall Achievement and the Cerebral Palsy Alliance scholarship. Roseanna began working at residential aged care facilities where her understanding of the need for suitable, person-centred equipment commenced. From there, she transitioned to work in community disability and quickly developed an interest for complex seating and mobility outcomes to benefit both the end user and wider network. She then stepped into a Team Leader role due to her passion for learning and best practice; supporting the Occupational Therapists with their own clinical needs and outcomes, and progressed to also provide external supervision to Occupational Therapists. Roseanna is motivated to support clinicians with their confidence and clinical reasoning allowing them to provide the best outcome for each individual user. Outside of work, Roseanna enjoys time with her dog, playing the 'cello, horse riding and aerial sports.
