Prescribing complex assistive technologies such as wheelchairs can be a long and stressful process for the therapist and the user. This may tempt therapists to consider the ‘delivery day’ of the wheelchair to be concluding this process. Is this realistic?
Friday 1st March was International Wheelchair Day, an annual day globally when wheelchair users celebrate the positive impact a wheelchair has on their lives. One of the wonderful things a well-prescribed wheelchair (including power-assist devices) can often facilitate is helping the user to live their life by improving their life-space mobility (mobility extending from within the home to beyond the town or geographic region). Whilst therapists may strive for their prescription to have a positive impact, some statistics show over 35% of all AT devices are abandoned^. There are numerous factors which may result in a new wheelchair or seating system limiting the user’s life-space mobility or be deemed a disappointment, to the point it may even be abandoned.
One of these factors is the progression of development of wheelchair skills, which are unlikely to be mastered on delivery day. Therefore, the day of delivery is not the end of the intervention. The amount of further input needed is likely to vary significantly depending on the user’s familiarity with, and complexity of, the provided AT. Let’s now look into some what’s, why’s and how’s of training.
What
Looking to the RESNA wheelchair service provision guideline, the final three stages are:
- Fitting/Training/Delivery
- Follow-Up Maintenance, & Repair
- Outcome Measures
Despite ‘training’ being included in the same stage as fitting and delivery, their guide does clarify that “Quantitative measures should be used to provide documentation of the training and follow-up services required after the fitting”. (pg.10).
The wheelchair service provision guideline then goes on to discuss what should be involved in ‘training’:
- Instruction in power or manual wheelchair mobility skills to optimize function and safety.
- Education regarding the set-up of the seating system including the specific postural support features and their impact on skin integrity, posture, function and overall health.
- Education regarding wheelchair parts management (e.g. removal and attachment of components), and care (proper charging, applying and disconnecting wheel locks) to insure maximum safety and positive long-term outcomes.
- Education regarding maintenance, follow-up, repair, and available resources including the funding coverage.
- Education and training specific to the integration of the wheelchair into the user’s lifestyle. This may include techniques for travel in accordance with known standards for wheelchair transportation (charging, folding, etc.), instruction in securing the wheelchair, occupant safety restraints when being transported in a motor vehicle, and safety (wheel lock and anti-tipper application).
Why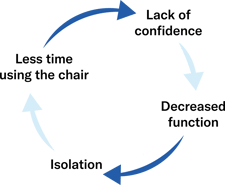
As a busy therapist it may be easy to question whether training is really so essential. In 2014, Brodie Sakakibara and his colleagues found that wheelchair skills accounted for over 90% of the direct effect of self-efficacy (being the user’s belief in their own ability to use a wheelchair in various situations) on life-space mobility. To say this another way, a user’s wheelchair skills have a huge impact on their confidence and competence using their wheelchair, which then has a strong influence on their community access.
How
Therapist
Once the basics of wheelchair set-up and maintenance have been provided, wheelchair skills training needs to be considered. There are many ways that wheelchair skills can be provided, and it may not be best provided by you! This might be a surprise to hear, but depending on your experience, and the user’s skills, it is important that you first identify what skills are necessary, and then who may be best to provide this training.
If you are looking to provide these skills, or educate others to then support the user, consider the content (what to teach), the techniques (how to teach) and the dose (how much, how often). These three factors should be considered in the intervention plan to meet the needs of the user and their supports to best facilitate progress.
Peer
It may or may not have crossed your mind to consider peer-led wheelchair skills training for wheelchair users. This may be formal or informal workshops or sessions where an adult wheelchair user would be the one providing the wheelchair skills training to your user, whether they might be an adult or child. There is increasing evidence for the benefits of this method including the credibility the peer has which may lead to more buy-in, opportunities for mentorship, and the observation of these skills in itself increasing self-efficacy.
If you aren’t aware of these being run locally, I would encourage you to consider whether you could be the person to make this change and facilitate meaningful skill development and vocational opportunities.
Other
There may be occasions where you or a colleague may not be able to provide this training, such as cost or time-limited environments, or user preference. This should not result in the user being discharged without any support or resources. Keep a list of other local services who may be able to provide this.
Another option is linking the user with an online resource, such as the Wheelchair skills program who also have their own YouTube channel with videos of the skills. This will provide the opportunity for the user to look up different skills, including explanations for how these are completed.
Author

Roseanna Tegel, BHthSc/ MOT
Clinical Services Specialist
Roseanna Tegel joined Permobil in May 2023 as a Clinical Services Specialist. She graduated from Western Sydney University in 2016 with a Bachelor of Health Science/Master of Occupational Therapy and received the Prize in Undergraduate Occupational Therapy for Overall Achievement and the Cerebral Palsy Alliance scholarship. Roseanna began working at residential aged care facilities where her understanding of the need for suitable, person-centred equipment commenced. From there, she transitioned to work in community disability and quickly developed an interest for complex seating and mobility outcomes to benefit both the end user and wider network. She then stepped into a Team Leader role due to her passion for learning and best practice; supporting the Occupational Therapists with their own clinical needs and outcomes, and progressed to also provide external supervision to Occupational Therapists. Roseanna is motivated to support clinicians with their confidence and clinical reasoning allowing them to provide the best outcome for each individual user. Outside of work, Roseanna enjoys time with her dog, playing the 'cello, horse riding and aerial sports.
.png)